Hiatal and Diaphragmatic Hernias
Hiatal Hernias
1st identified on post mortem examinations in 1903 Radiographically in 1926
10% of population have hiatal hernias
Congenital and Acquired factors:
extracellular matrix, higher intra-abdominal pressures, inherent weakness of diaphragm tissue
RF: F>M (2:1), Older, Obese
Symptoms: GERD, Dysphagia, Post prandial pain, Dyspnea (depending on degree), Chest pain (depending on degree), fullness, anemia (up to 1/3 of patients)
Dx: X Ray, Swallow Study, EGD, CT
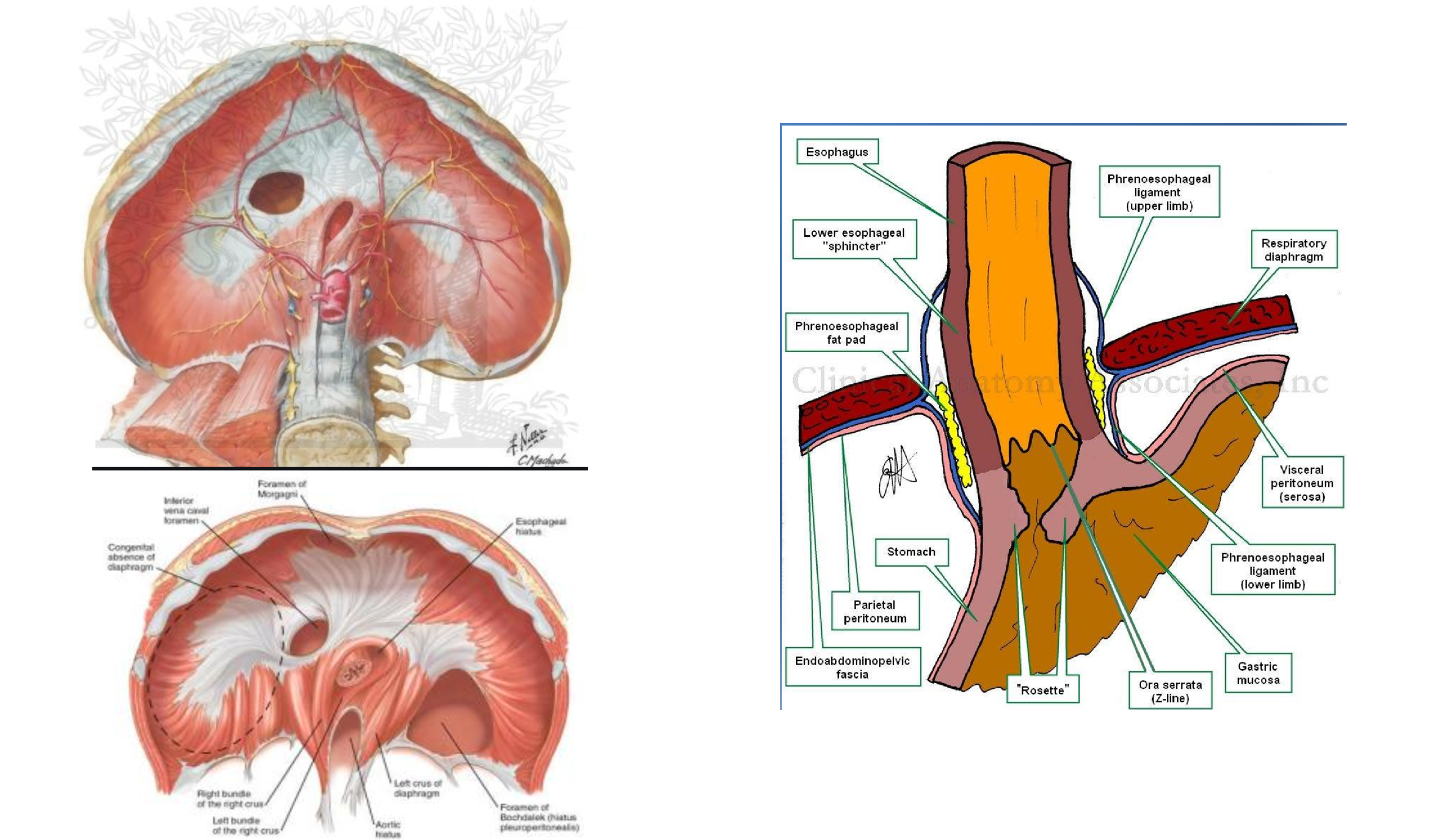
General Diaphragmatic and Hiatal Anatomy
Principles of Surgical Repair
-Complete reduction and excision of hernia sac
-Reduction of herniated stomach AND 2-3 cm of esophagus in abdomen
-Repair of diaphragmatic hiatus
-Fixation of stomach into abdomen OR Fundoplication
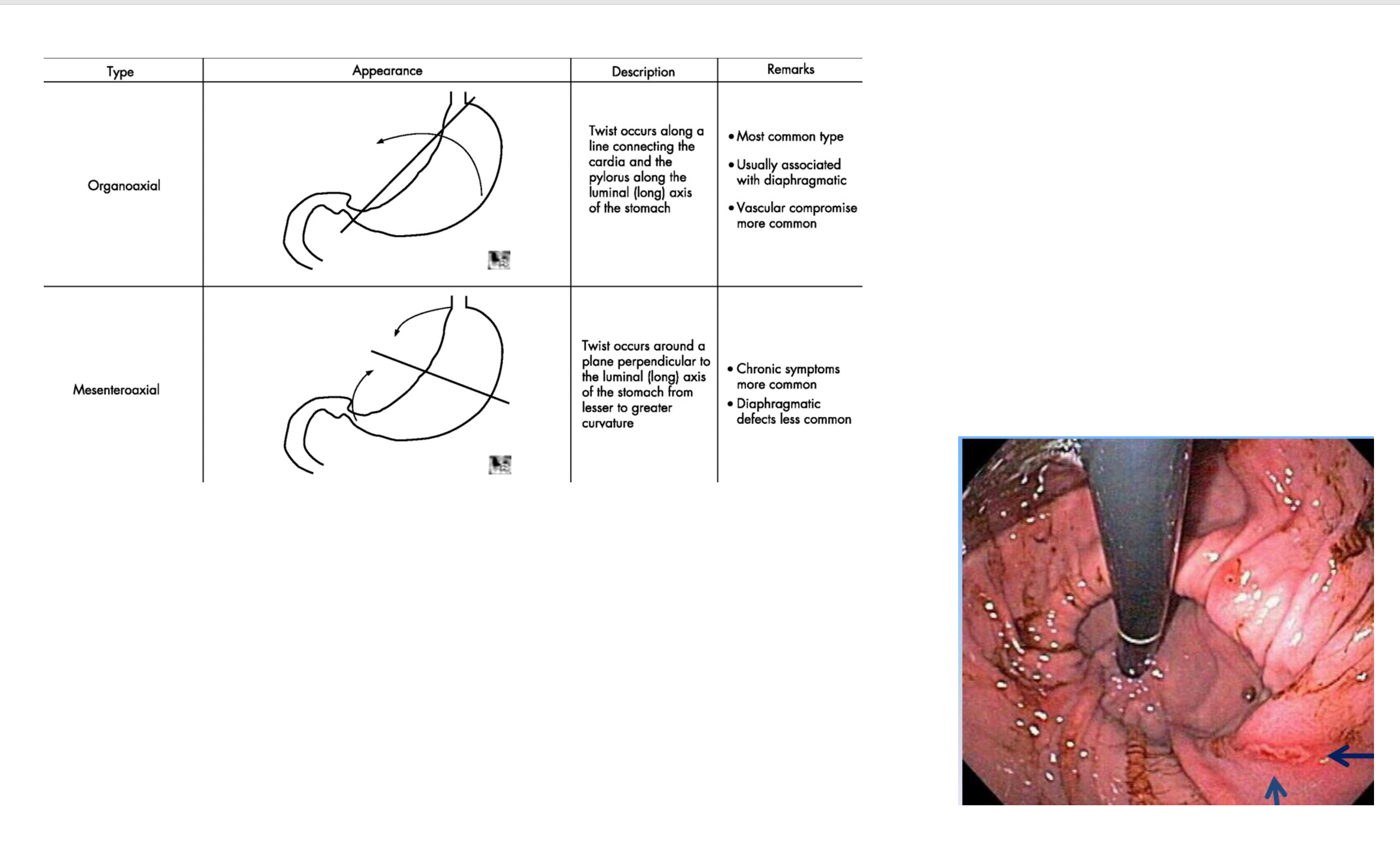
Image 1: Types of Volvulus from diaphragmatic hernias
Image 2: Can you name this type of ulcer?
General Conduct of the Operation
-Position/ Pre-op (+/-EGD)
-Entry into the abdomen, liver retraction
-Reduction of hernia and its contents
-Crural Dissection
-Assessment of esophagus
-54F Visigi
-2-3cm of esophagus in abdomen
-Crural Repair (Interrupted non-absorbable suture)
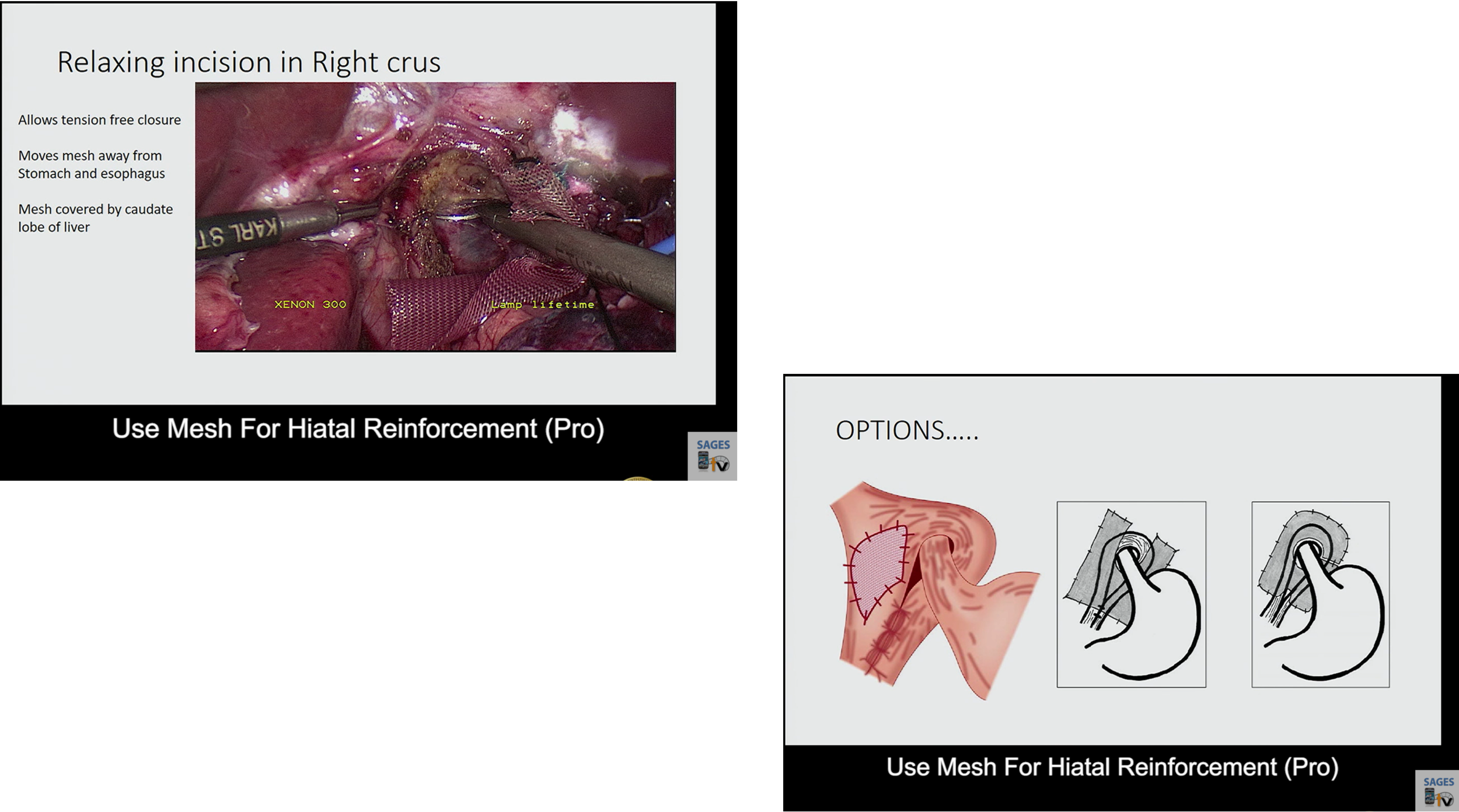
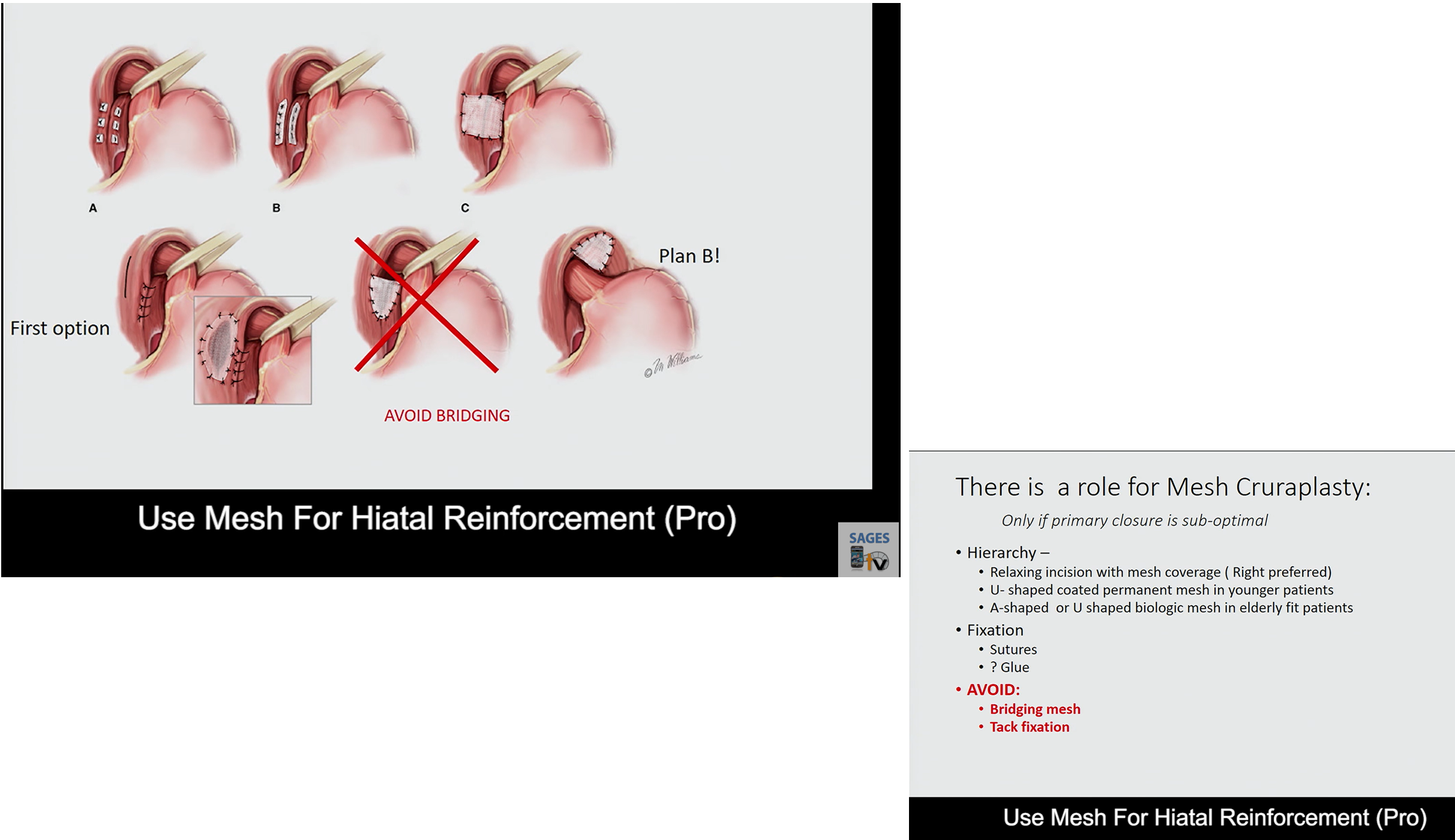
-Rarely use mesh (should not bridge; should be to reinforce)
-Relaxing incision (full thickness, right crus)
-Fundoplication vs Fixation
To mesh or not to mesh?
Why not mesh?
No good RCT
Recurrence rate at 5yrs is the same
Meta-analysis don’t show any benefits
either
Concern for erosion/ infection/ migration
When mesh?
Fragile crura
Re-do surgery after failed primary cruraplasty
Round or Globular Hiatus
COMPLICATIONS
Esophageal Perforation
Splenic Injury
Vagus Nerve Injury
Recurrence