Abdominal Aortic Aneursym
Abdominal Aortic Aneurysm
Normal caliber: 2-3cm
MCC: atherosclerosis (medial layer degeneration)
RF: M (4-8% have an occult AAA), smoking (higher risk of rupture, and faster expansion), older age (>60), fam history
Most are asymptomatic.
If they do have symptoms: back pain, abdominal pain, compressive symptoms, hypotension
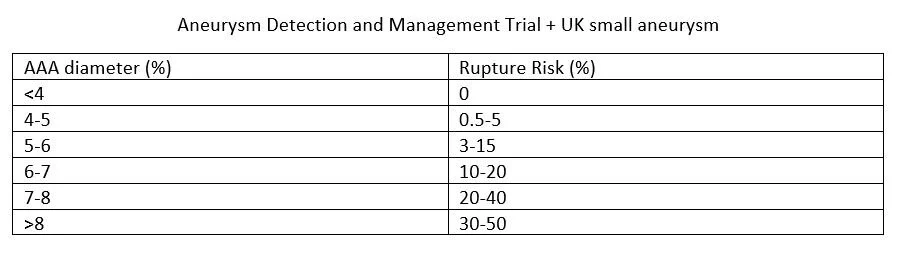
Increasing incidence 2-10x (large vs small aneurysm)
*20% have fam history
*40% of AAA associated with iliac artery aneurysms
Risk Factors for infection:
arterial injury (IV drug/trauma/iatrogenic)
antecedent infection, impaired immunity
Staph Aureus is most common (28-71%), Salmonella is next (15-24%)
May see peri-aortic air
Vanc empirically. Then can use ceftriaxone, fluoroquinolone, zosyn
Repair indications:
>5.5cm for average male patient
>5cm for females
Growth >1 cm/yr
Infected (mycotic)
Becomes symptomatic
Mortality w/ elective repair 2-4%
Mortality in emergent cases 30-70%
Urgent repair
- Evidence of distal emboli
- Known aneurysm that has become tender
- Abdominal/back pain
Pre-op evaluation
Measuring A/P > lateral
Consider landing zone (proximal and distal) length, diameter, and tortuosity
Management of ruptured aneurysm
- Rapid transport
- Resuscitation
- Permissive hypotension to SBP 90-100
- Emergent OR
- Maintain temp >33C (lower causes capillary leak syndrome)
- Consider intra-aortic balloon control
- Supraceliac and distal control
- Inspect for organ viability and limb perfusion
Management Options:
Open vs EVAR
5% vs 1.5% mortality
But more surveillance + future procedures; Need right type of anatomy; capabilities of facility
OPEN
Transabdominal or reptroperitoneal
- If extending to renals/ suprarenal may benefit from transabdominal
- Proximal and distal control
- Heparinize w/ 100U/kg +/- mannitol. Let circulate for 5 min
- Open aneurysm, clear thrombus, suture back bleeding lumbars
- Suture to healthy aorta
*** if w/ evidence of infection, need to resect portion
- Use sac to isolate graft from intestine
ENDOVASCULAR
EVAR accessed via sheaths, typically using both femorals. A 16F and 8F sheath are typically needed
COMPLICATIONS
Aortoenteric fistula
- 6mo after surgery
-hematemesis, hematochezia
- around 3rd/ 4th portion of duodenum
- bypass around non-infected field, resect graft, close duodenal defect
Mortality
- early: 2/2 MI; late: 2/2 renal failure
- RF: Cr >1.8, CHF, EKG, ischemia, pulm dysfunction, age, female
Bleeding
Graft thrombosis
Impotence from autonomic disruption
Vein injury
Pseudoaneurysm
Atherosclerosis
Bowel Ischemia- typically middle and distal rectum spared
Graft Infection
- 1% (typically w/ staph epidermidis; also staph aureus, and E Coli)
- fluid, gas, thickening around graft
- cultures typically negative
- want to bypass around non-infected field (ax-fem; fem-fem)