Gastro-Duodenal Ulcers
“Unfortunately, only a small number of patients with peptic ulcer are financially able to make a pet of an ulcer.” - William James Mayo
Peptic Ulcers
H. pylori infection is the number 1 risk factor for peptic ulcers
•MCC: H. pylori, followed by NSAIDs
•H. Pylori Tx – PPI, Amoxicillin with Clarithromycin or Metronidazole (‘CAP’ or ‘CAMO’)
•Confirm eradication with urea breath test
•Presents with bleeding – ALWAYS EGD with some adjunct
•Indications for surgery: perforation, bleeding despite endoscopic therapy, obstruction
Other Ulcer Types:
Cushing – Severe head trauma, due to increased gastrin and HCl hypersecretion// How to remember
Cushing was neurosurgeon, Head trauma – Cushing ulcer
Curling - 30% TBSA Burns, due to mucosal ischemia //
How to remember:Curling Iron Burns – Curling ulcer
Cameron’s -typically linear ulcerations by the GE junction, secondary to a diaphragmatic compression on the stomach. Occurs in the setting of a hiatal hernia
Marginal Ulcer- ulcer’s found in the gastro-jejunostomy, typically secondary to lack of Brunner’s glands in the Jejunum
It’s bleeding!
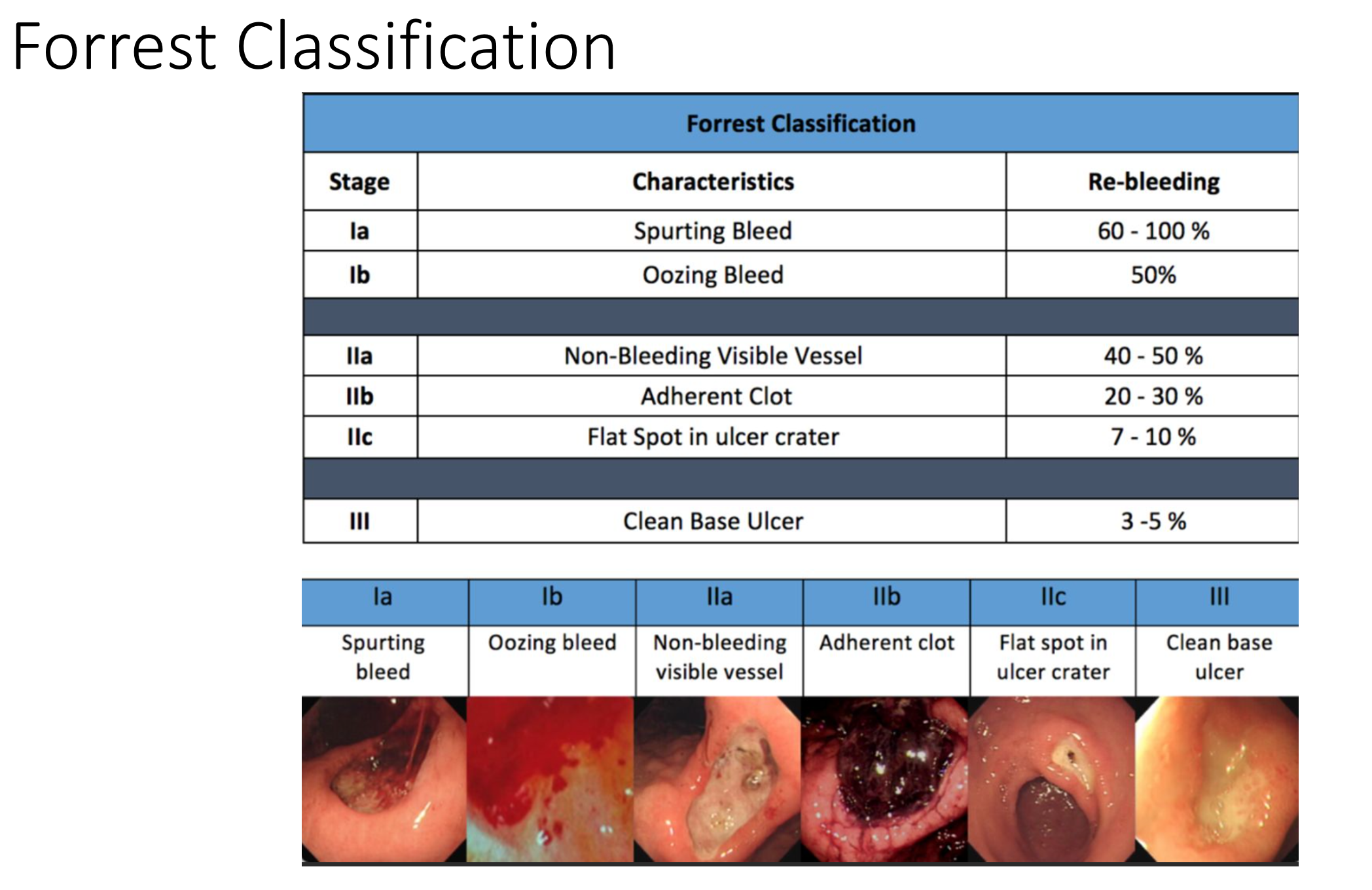
•Dx/Tx: reverse anticoagulation, EGD w/ adjuncts
•Active pulsatile bleeding and visible vessel are highest re-bleeding risks
•If liver failure and from esophageal varices --> EGD w/ banding, TIPS if local therapy fails
•If unable to find source --> angiography --> tagged RBC scan
•Gastric varices w/o esophageal varices – hx of pancreatitis – think splenic vein thrombosis. Dx with US. For symptomatic pts ---> splenectomy
Surgical Options:
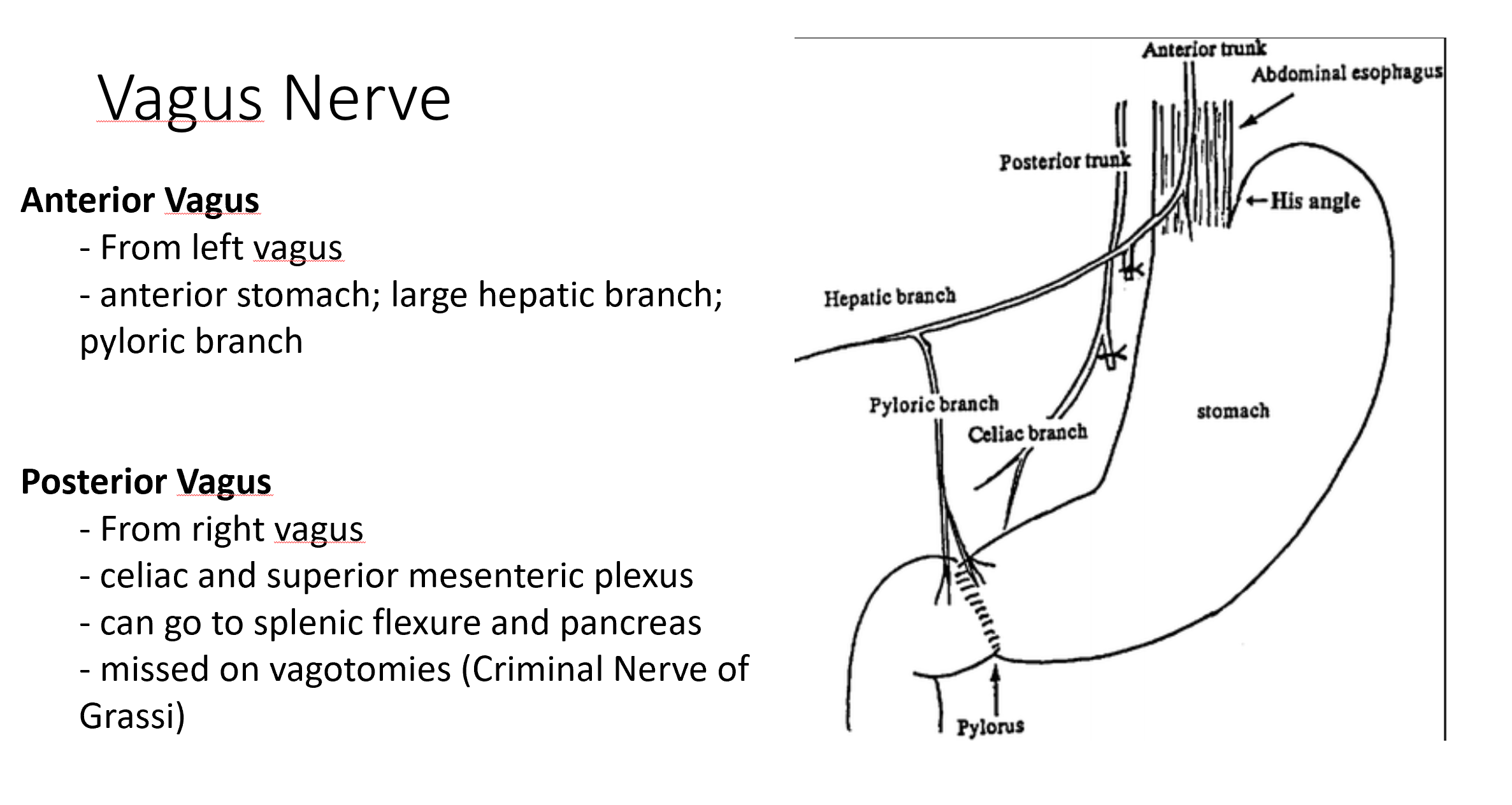
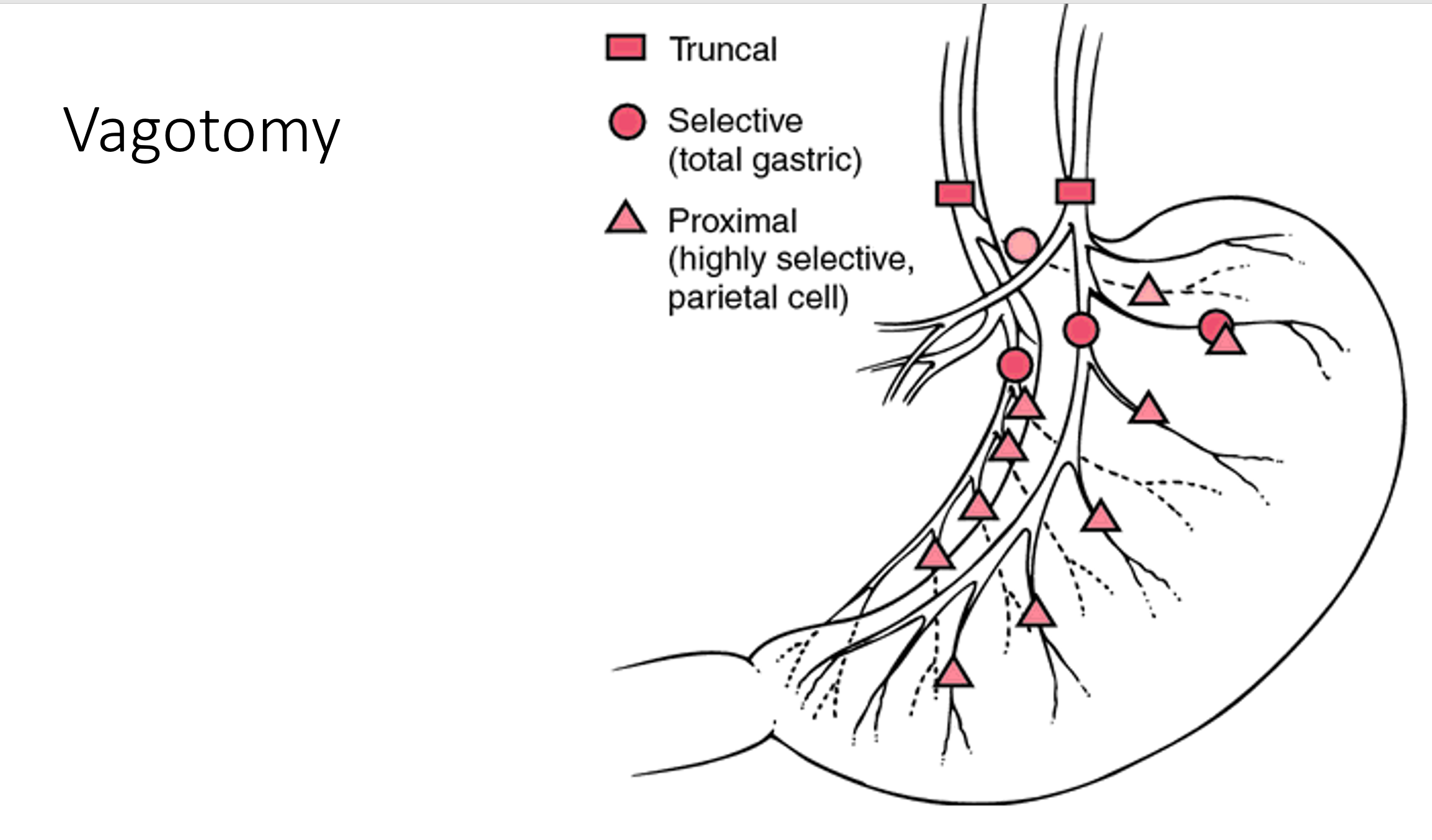
•Perforated GASTRIC ulcer- antrectomy
with truncal vagotomy (RISK OF GI CA)
•Perforated DUODENAL ulcer – graham
patch or if bleeding duodenotomy w/ GDA ligation
•Highly selective vagotomy – highest ulcer
recurrence rate
•Best reconstruction is RY – less dumping
syndrome and bile reflux
•Always send ulcer tissue to path