Chronic Limb Ischemia Part 3
Surgical Management of Aorto-iliac, Femoropopliteal
and Tibioperoneal Disease
Aorto-Iliac Disease:
-Identify suitable level
-location of renals
-end-to-end if possible: better in-line flow, easier closure of retroperitoneum, decreased infection/fistula rates/esp if w/ aneurysm
***will need patent external iliacs for above as this will allow for pelvic blood supply
IF w/o patent external iliacs- end to side anastomosis. Forward flow will continue to perfuse pelvis
Steps:
Expose femorals via b/l oblique incisions (expose to inguinal ligament)
Control inferior epigastrics and circumflex iliacs
Dissect to superficial and deep femoral arteries. Determine if endarterectomy/ patch is required. Get vascular control
Expose abdominal aorta via midline, transperitoneal incision
Ligament of treitzà mobilize duodenum
Proximal control (depending on level of disease may be supraceliac, through gastrohepatic ligament)
Proximal endarterectomy, then quick flash. Aim for as close to renals as possible to prevent progression to remnant infrarenal neck
Distally, identify a soft landing spot. APPROACH LATERALLY to prevent nerve injury (sweep these upwards)
Minimize dissection to prevent injury to iliac veins, hypogastric plexus, and presacral nerves (travel ANTERIOR; impotence, premature ejaculation)
Tunnel to the groin. Proceed directly anterior to vessels to avoid ureteral injury
Identify proximal landing zone
Heparinize
Excise portion of aorta (2-4cm) superior to IMA (allows for back bleed). Oversow or staple end of aorta. If not excising, identify soft region for side anastamosis.
Use 3-0 prolene
Create distal anastomosis (end or side).
Use 5-0 prolene
Close
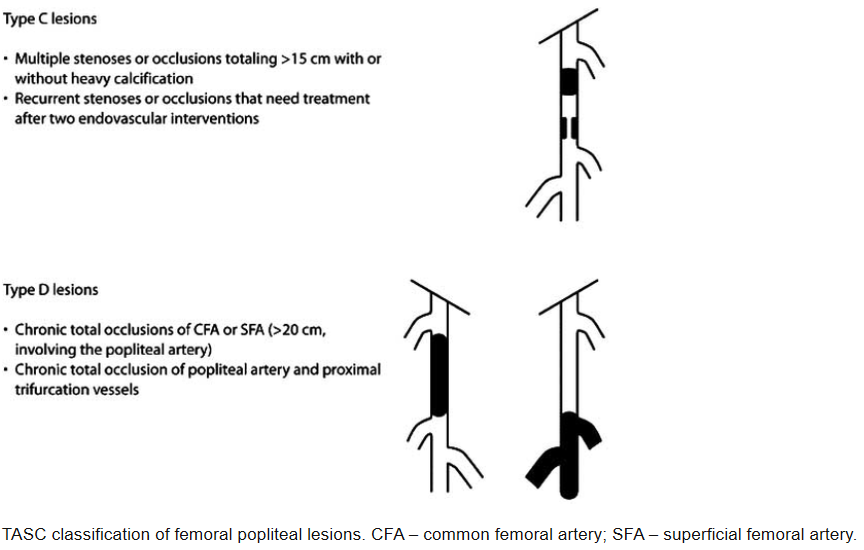
Femoropopliteal Occlusive Disease:
Bypass is the gold standard, but depends on comorbidities, long term prognosis, severity of disease, location
*BASIL trial, in patients that live >2 years, bypass was superior to stenting alone
* Bypass principles: Good inflow. Good outflow. Good conduit
Steps:
Vein identification/harvest (clamp at SFJ proximally, ligate tributaries away from main vessel w/ silk sutures, hep-saline flushes)
Proximal and distal control
Proximal: CFA. Dissect to inguinal ligament// Profunda and SFA also controlled w/ silastic loops. Vein is posterior to this
Distal- can be above or below knee
Above knee: medial thigh, anterior to sartorius. Dissect between vastus medialis and sartorius. Dividing adductor fascia exposes AK popliteal
Below knee: 1 finger breadth posterior and medial to the tibia. Dissect through posterior fascia and identify gastrocnemius.
Enter fascial sheath and separate vein from artery
Tunnel
Heparinize
Arteriotomy, endarterectomy
Anastomosis with double armed 5-0 or 6-0 prolene
Assess patency
Closure
*** Endarterectomy- longitudinal arteriotomy. Close with saphenous vein/bovine pericardium patch.
GRAFT LOSS w/in 30 days -> technical error
w/in 1-2 years -> intimal hyperplasia
Tibioperoneal Occlusive Disease:
Balloons typically 1.5-4mm in size
Inflate over 1-3 minutes. Can hold for 3-4 minutes
Proximal- typically at CFA.
Distal- ideally posterior or anterior tibial as this has inline flow to arterial arches of the foot
Posterior Tibial/ Peroneal
2cm posterior medial to tibia. Incision begins below the knee joint and goes 10-15cm
Dissect down gastroc proximally/ soleus midway/ posterior to malleolus distally. Retract medial head posteriorly. This should expose popliteal fossa
Anterior Tibial
Incision is between tibia and fibula. Incise tibialis anterior and extensor digitorum longus
Tunnel
Heparinize
Anastamose w/ 5-0 or 6-0 prolene sutures
Complications:
Infection (up to 15%)
Cardiac complications
Ureteral injury
Graft thrombosis (5-30%)
Reperfusion injury
Steal syndrome
Emboli: Spinal cord ischemia, Bowel ischemia, Digital Ischemia