Chronic Limb Ischemia (part 1)
Signs of peripheral artery disease:
Pallor, rubor, hair loss, slow capillary refill.
Claudication
Pain, Ulcers
Claudication is a supply-demand phenomena. Can be described as cramping, aching, or fatigue. Less likely it is described as weakness
#1 preventative- statins
Other RF: smoking (offer cessation support), homocystinuria (folate, B12)
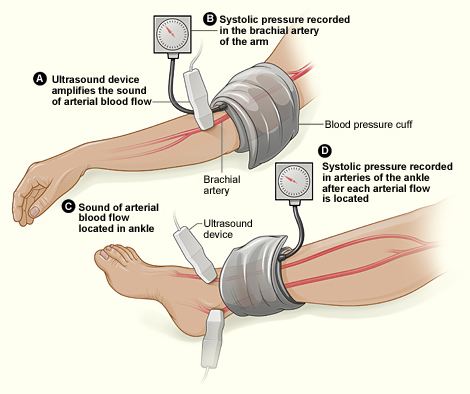
Ankle-Brachial Index
Take the higher of the brachial, and higher of of the ankle pressures
Ankle Brachial Index (ABI)
0.9-1.2 normal
<0.9- claudication
0.4-0.7 rest pain (calf/foot)
<0.4- ulcers
<0.3-gangrene
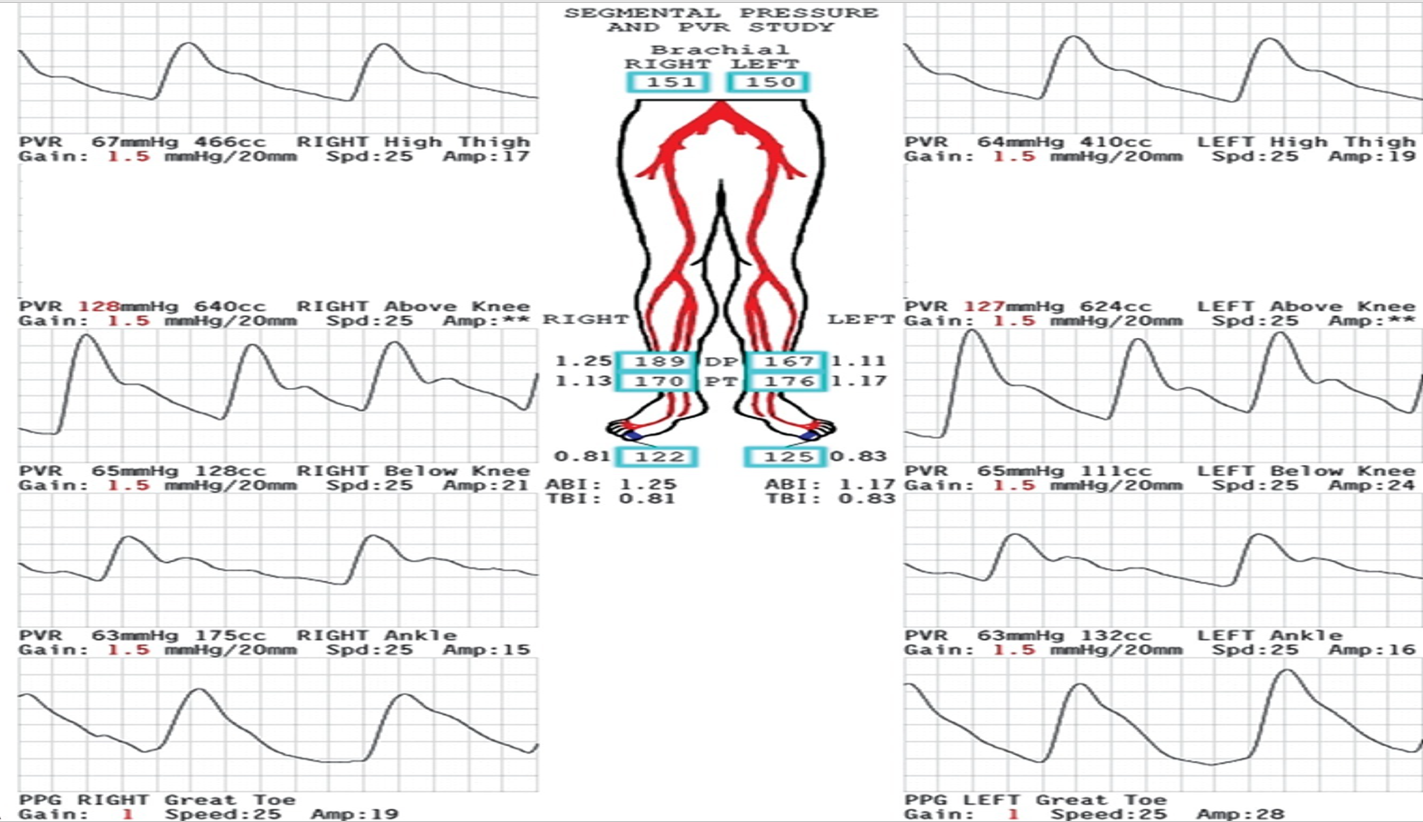
Symptoms occur below level of occlusion:
Buttock- aortoiliac
Thigh- external iliac
Calf- Common femoral/Proximal superficial femoral
Foot- Distal superficial femoral/popliteal
DX:
ABI
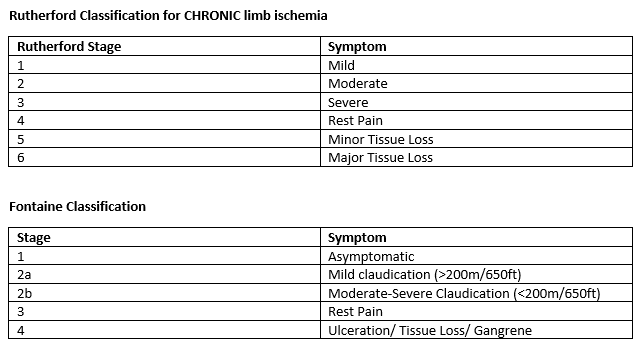
PVR (pulse volume recordings)- identify level of lesion
CTA, Angiogram
Duplex- good for surveillance
Medical Management:
HTN- Goal SBP <140 for non diabetics, SBP<130 for diabetics
DM2- Goal A1c <7
Statin- decreases cardiac events and can help decrease claudication symptoms
Aspirin
Cilostazol- phosphodiesterase inhibitor -> vasodilate + smooth muscle relaxant + decrease platelet aggregation
Exercise
Medical therapy first (aspirin, statin, walk until with pain -> walk)
***lumbar stenosis may mimic claudication
look for multiphasic readings
want toe pressures of >35 mmHg
want amplitudes >30
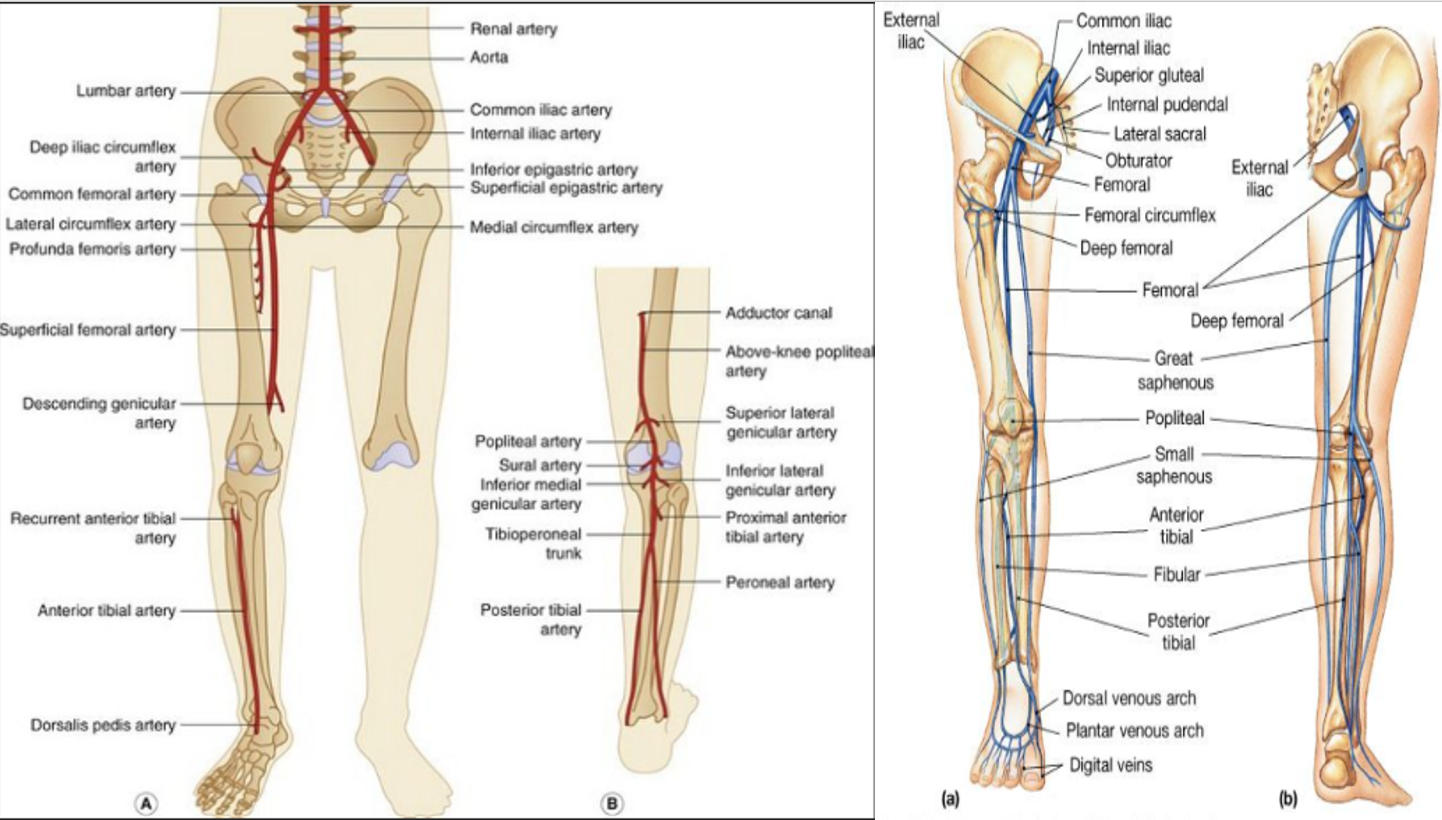
Vascular Anatomic Review
Indications for surgery:
rest pain, ulceration, lifestyle limiting, acute emboli
——————————————————————————————————————————————————————————————————————————————————————————————————————————————————————————————————————————————————————————————————————
-lesion is at aortic bifurcation or above
-TX: aorto-bifem graft
MC atherosclerotic occlusion is at Hunter’s Canal (distal SFA; sartorious runs over this)
***Collaterals: circumflex iliacs, circumflex femoral, geniculate