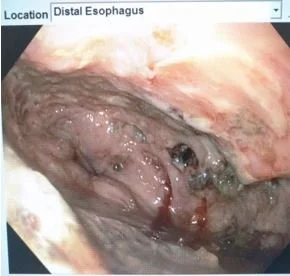
Esophageal Perforation
Etiology:
>50% iatrogenic
15% “Spontaneous”
12% Foreign Body
9% Trauma
2% Intraoperative
1% Malignancy
MACKLER’s triad- Subcutaneous emphysema, vomiting, and chest pain
But regardless of the cause, esophageal perforation is a surgical emergency
Mortality:
Cervical- 6%; Thoracic- 34%; Abdominal- 29%
Overall: 14-18%; Significantly increases with delays
**Spillage can cause necrotizing inflammation which ultimately leads to sepsis, multiorgan failure, and death
Key Anatomic Regions:
Cricopharngeus
Broncho-aortic region
Esophago-gastric region
*Killian’s triangle- natural area of weakness over posterior esophageal muscularis. Cricophargeous and Oblique inferior constrictors
Diagnosis:
History/ Physical Exam- vomiting, trauma, ingestion, chest pain// crepitus
Chest X-Ray - Pneumomediastinum, Subcutaneous Emphysema
Esophogram - gastrograffin, dilute barium
CT Chest
Diagnose, Stabilize, Treat
Greater than 24hr delay near doubles mortality (European Journal of Cardiothoracic Surgery; Diseases of the esophagus)
Operative management will be required for a majority of perforated patients
Management
NPO
Large Bore IVs
Antibiotics (Pip/Tazo; Carbapenems; Clindamycin +Fluoroquinolones +/- Antifungals)
Intensive Care Management
For a majority of esophageal perforations, primary repair is the optimal management strategy
Exceptions:
Cervical perforations w/ difficult access and is drainable
Diffuse mediastinal Necrosis
Defect is too large
Pre-existing esophageal disease
Unstable patient
Principles:
Debride devitalized tissue
Incise muscle fibers superior and inferior to injury
Close mucosa w/ absorbable suture, and muscularis with non absorbable
Vascularized pedicle flap (intercostal, serratus, lat dorsi, diaphragm)
Cervical Perforation
Left sided approach UNLESS clearly visualized defect on right side
Incision made over lower 1/3 of sternocleidomastoid
Mobilize SCM and Carotid Sheath laterally/ Trachea and Esophagus Medially
*can divide middle thyroid and omohyoid
Irrigate and leave a drain, or allow to close via secondary intention
Thoracic Perforation
Right sided approach if high thoracic (T6/7 and above)
- via 6th or 7th rib posterolateral thoracotomy
Left sided approach if low thoracic (T8 and below)
- via 7th or 8th posterolateral thoracotomy
Open up muscularis to reveal entire extent of perforation
Two layer repair (inner absorbable, outer non absorbable) +/- flap
Prepare pedicle flap early
Evacuate Pleural Space
Isolate perforation using a penrose drain
Place chest tubes
***bail out- cervical diversion, irrigation, drainage, return when patient more stable
Stenting:
Extensive comorbidities
Advance mediastinal sepsis
Large defects
Inability to tolerate more extensive surgery
***higher risk of failure if: cervical, GE junction, perf >6cm, persistent leak
***want to remove stents ideally <4weeks
***stents should be placed by experienced clinicians/ decision to do so by multidisciplinary team
Endoluminal Sponges also now coming into play
Post-Op:
ICU
ABX
Nutrition consideration
Consider Esophogram (5-7 days later)