Carotid Artery Stenosis
Risk Factors:
Smoking, HTN, DM, Hereditary factors
Plaque tends to build up over the bifurcation given the change in flow and caliber of the vessel
Symptoms:
Focal Neurological Symptoms
Myocardial Infarction is typically the leading cause of morbidity in surgical repair; neurologic complications is the second cause f morbidity
Initial Management:
Medical management- Aspirin, statin, blood pressure control, smoking cessation
*Aspirin reduces stroke risk
*Statins may be associated with improved outcomes and symptomatic patients (lower mortality and ischemic stroke)
Indications:
NASCET Trial
Bottom Line Up Front:
Symptomatic patients with >50-69% stenosis had a 29% reduction in 5yr risk of death or stroke
The benefits for those with >70% stenosis were so great that they stopped the trial early
*Rate of ipsilateral stroke is 26% and medical group versus 9% surgical group. Absolute risk reduction of 17%. Number needed to treat 7-8 patients
ACAS Trial
Bottom Line Up Front:
ASYMPTOMATIC patients with >60% stenosis had a 5.1% risk vs 11.0% risk of ipsilateral stroke, with a 57% reduction in TIA/Stroke over 5 years
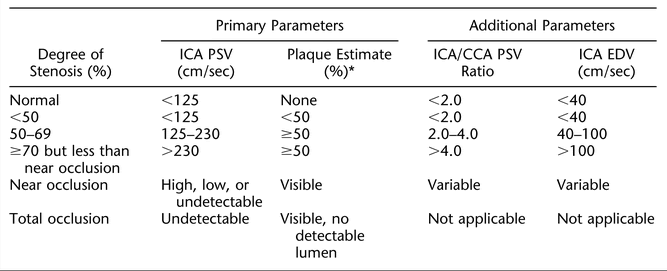
Diagnosis:
Ultrasound, MRA, CTA, Angiography,
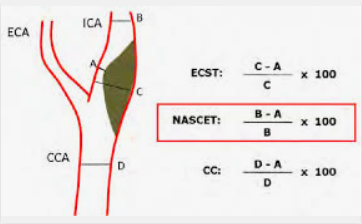
ECST = European Surgical Carotid Trial
NASCET = North American Symptomatic Carotid Artery Trial
Absolute Contraindication: Complete occlusion
Relative contraindication: Prior irradiation, tracheostomy, prior radical neck dissection, contralateral vocal cord paralysis, atypical lesion location, recurrent severe carotid disease, high medical risk
Risk factors for complications: Greater than 70-80 years old, severe heart disease, severe pulmonary dysfunction, renal insufficiency, stroke is indication for surgery, abnormal anatomy
Complications:
MI, Stroke, Restenosis, Bleed, Hypertension (2/2 baro-receptor manipulation)
Nerve injuries:
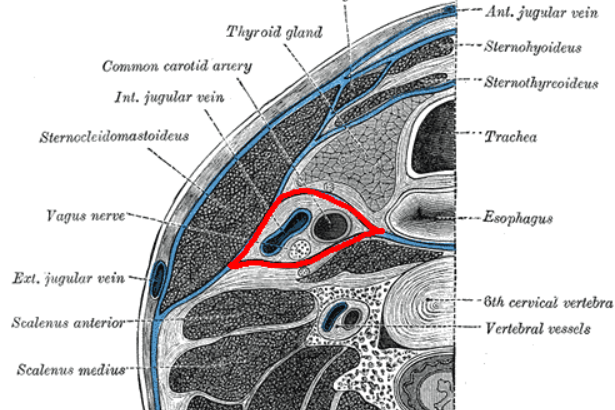
Vagus nerve injury – MC injury; from vascular clamping. GET HOARSENESS
Hypoglossal- tongue deviate to injured side. Affect speech and mastication
Glossopharyngeal- difficulty swallowing
Ansa- strap muscles, no real deficit
Mandibular branch- affects corner of mouth
An alternative to patients with prior neck surgery, neck radiation, prohibitive surgical candidates is carotid artery stenting.
According to the CREST trial, this is associated with similar rates of stroke, MI, and death
GENERAL CONDUCT OF THE OPERATION:




1) Position the patient facing away from the affected side. Consider a shoulder role
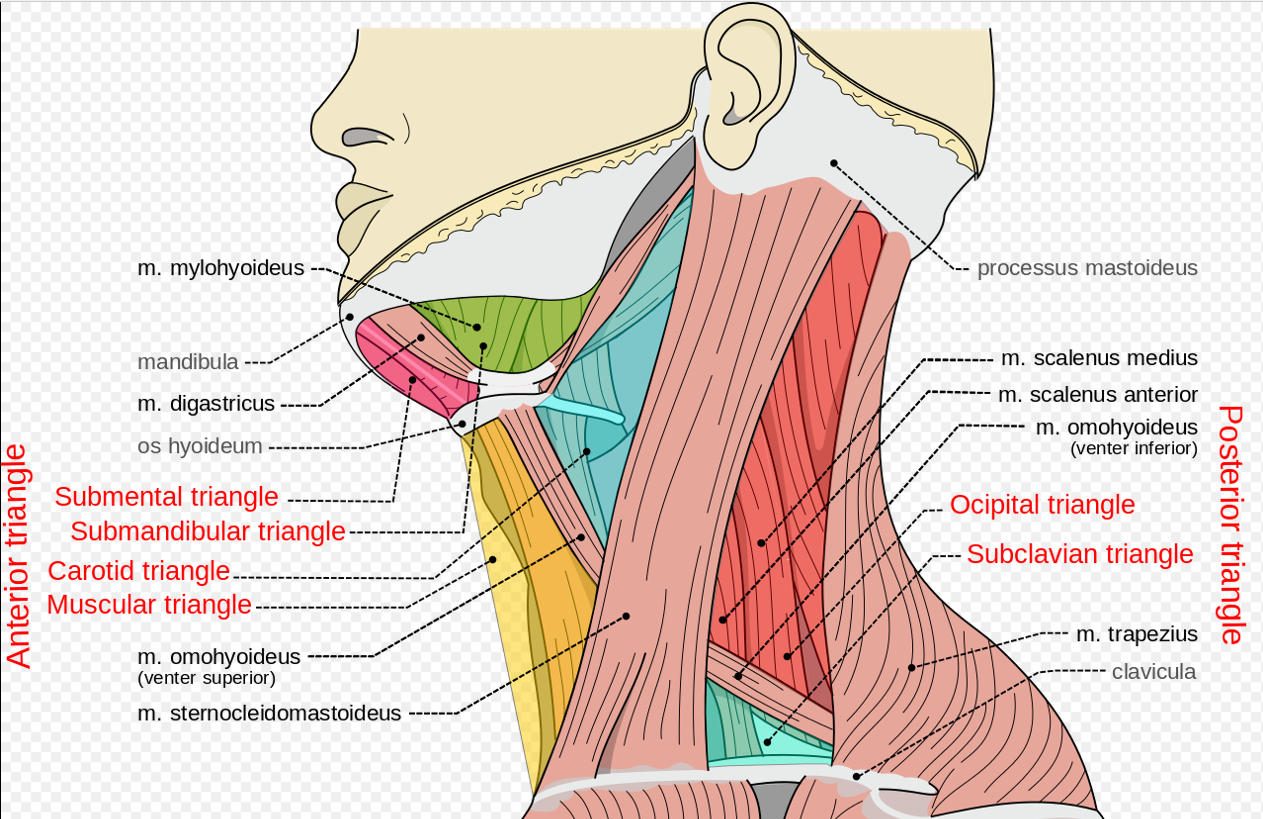
2) Make an incision along the anterior border of the sternocleidomastoid, and dissect down to the level of the carotid sheath
*carotid sheath contains the IJ, Carotid Artery, and Vagus Nerve
3) Isolate the Carotid Artery
4) Prepare to clamp (can use rumel clamp, vascular clamps, etc). The circle of willis should have been assessed for patency prior to this)
* If not an “always shunter,” Use a shunt if back pressure is <50mm Hg or if the contralateral side is tight
* heparinize the patient
5) Shunt in ICE (internal, common, external). Remove at end of case in OPPOSITE ORDER
6) A longitudinal arteriotomy is performed below the level of the bifurcation and extended proximally and distally
The plaque is typically located at the carotid bifurcation and at the origin of the internal carotid artery.
7) The intima and media are removed. Ensure a good distal end point. May need to be tacked down
8) back bleed/ flush
9) Patch may be used to avoid strictures. Materials include polyester (Dacron), and PTFE, and bovine pericardium. There is some evidence that points to improve on both cysts, lower stroke rates, and later restenosis.
10) Ultrasound. Close. Perform an immediate neuro exam